| Childhood Allergy and the NeOnatal Environment |
CANOE |
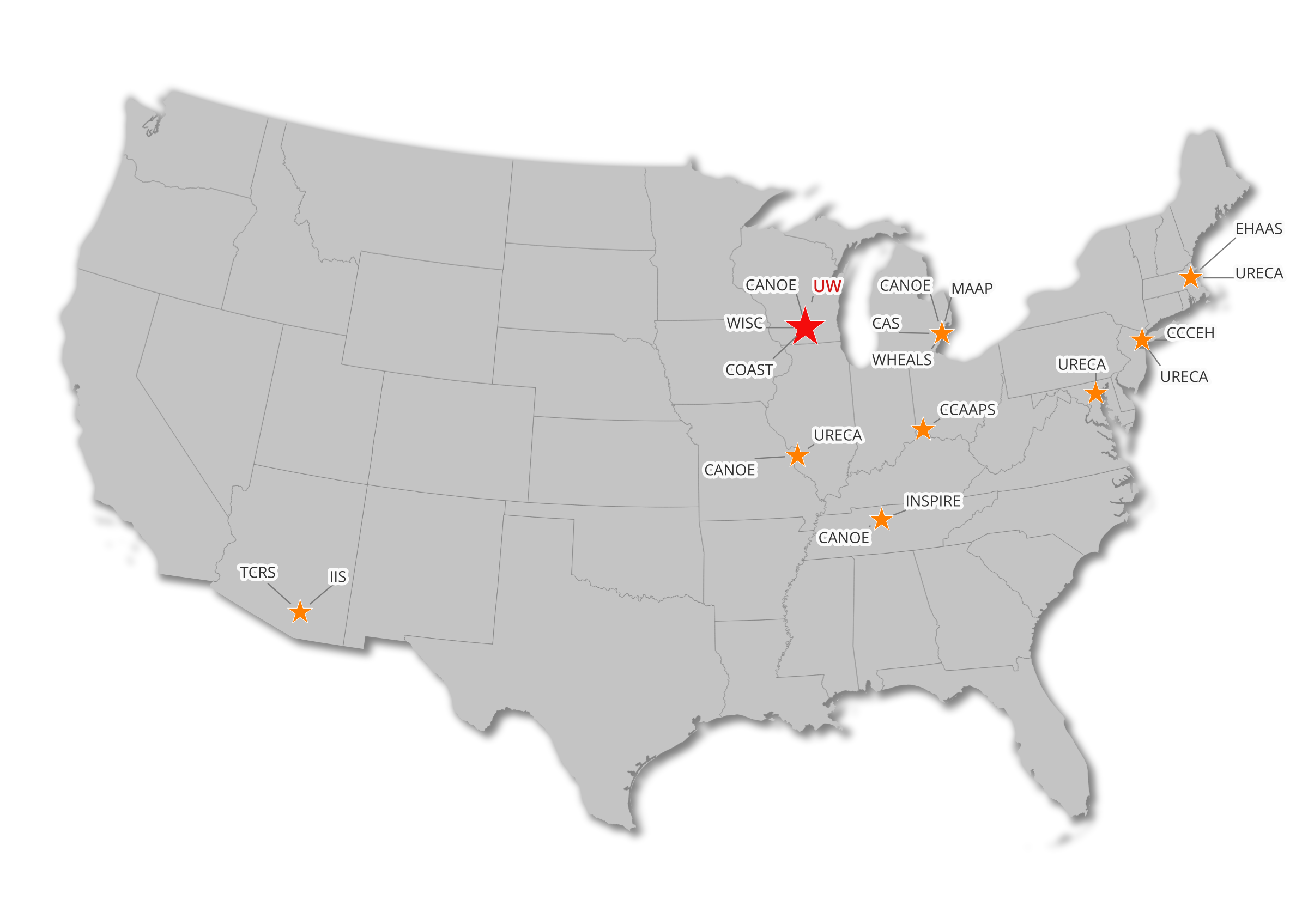
The Childhood Allergy and the NeOnatal Environment (CANOE) study led by Anne Marie Singh is a birth cohort established in 2021 under the NIH Environmental Influences on Child Health Outcomes (ECHO) Program, utilizing multi-omics (transcriptomics, genomics, epigenomics, and microbiomics) approaches to investigate how environmental exposures influence airway epithelial gene expression and asthma development, beginning with nasal airway cells obtained within days after birth. The CANOE cohort (478 families) was recruited in four US cities and has broad representation for demographics, geography, and exposures. |
539 |
Anne Marie Singh |
Detroit, MI; Madison, WI; Nashville, TN; St. Louis, MO |
| Childhood Allergy/Asthma Study |
CAS |
The Childhood Allergy/Asthma Study (CAS), initiated in 1987 by Dennis Ownby and also led by Christine Johnson and Edward Zoratti (Henry Ford Health, Detroit MI), is a population-based study of general-risk children (n=835) in a suburban area north of Detroit. The main goal of the study was to identify early life exposures, including allergens, pets, and tobacco smoke, which influence asthma development. Data collected include perinatal medical record abstraction, home characteristics and exposures, and samples of home dust and air, urine, cord blood, and child and parental peripheral blood. Clinical information included pulmonary function, methacholine challenge, exhaled nitric oxide (eNO) and IgE measurement and allergy skin prick tests (SPT). DNA and urine samples have been banked. |
835 |
Dennis Ownby, Christine Johnson, Edward Zorrati |
Detroit, MI |
| Childhood Origins of Asthma |
COAST |
The Childhood Origins of Asthma (COAST) study led by Robert Lemanske Jr. and Daniel Jackson (University of Wisconsin–Madison) is a high-risk (parental history of asthma and/or allergy) birth cohort (n=289) established in 1998 to evaluate the contribution of both genetic and environmental (with emphasis on respiratory tract infections) factors in early life on the development of childhood asthma and allergic diseases. Environmental assessments in early life include extensive viral diagnostics, pets, household characteristics, and dietary information. Extensive phenotyping data include airway physiology (spirometry, impulse oscillometry, eNO, and mannitol bronchoprovocation), airway imaging, immune function (cytokine response profiles, allergic sensitization, both developmentally assessed since birth), genotyping (including epigenetics), and the microbiome. |
285 |
Robert Lemanske Jr. and Daniel Jackson |
Madison, WI |
| Cincinnati Childhood Allergy and Air Pollution Study |
CCAAPS |
The Cincinnati Childhood Allergy and Air Pollution Study (CCAAPS), led by Patrick Ryan and Neeru Hershey (University of Cincinnati) and started in 2001, is a longitudinal cohort of children (n=762) born to atopic parents in greater Cincinnati, OH. The objective is to determine if exposure to traffic-related air pollution (TRAP), specifically diesel exhaust particles (DEP), is associated with the development of allergic disease and asthma and if this association is modified in a genetically at-risk population. Exposure to multiple environmental stressors has been assessed prenatally throughout childhood for all study participants and includes TRAP, allergens, mold, tobacco smoke, housing and community characteristics, and others. Other assessments include SPT, spirometry, eNO, and methacholine challenge testing. Biologic samples include blood, urine, saliva, DNA, toenails, teeth, and hair. Exposure assessments include TRAP, indoor/outdoor allergens, mold and data from geographic information systems. |
763 |
Patrick Ryan and Neeru Hershey |
Cincinnati, OH |
| Columbia Center for Children’s Environmental Health Cohort |
CCCEH |
The Columbia Center for Children’s Environmental Health Cohort (CCCEH), led by Julie Herbstman (Columbia University, NYC) and Rachel Miller (Mount Sinai, NYC) and established in 1998, is a birth cohort of participants (n=727) living in Northern Manhattan and the South Bronx of New York City. The main goals are to undertake a comprehensive community-based assessment of environmental risks to African American and Latino infants and children living in Manhattan and to develop strategies for reducing and ultimately preventing those risks. The focus of environmental assessments includes TRAP, allergens, housing characteristics, and endocrine disrupting chemicals. Clinical information gathered on the children includes SPT, repeat IgE levels and lung function tests. DNA, serum, and urine samples have been banked. |
727 |
Julie Herbstman and Rachel Miller |
New York, NY |
| Epidemiology of Home Allergens and Asthma Study |
EHAAS |
The Epidemiology of Home Allergens and Asthma Study (EHAAS) led by Diane Gold (Harvard University, Boston MA) is a high-risk (parental asthma and/or allergy) birth cohort (n=505) from Greater Boston established in 1994. EHAAS evaluates influences of early-life indoor home exposures to allergens, fungi, and microbial components on the development of wheeze, asthma, lung function, and related immune responses (e.g., allergic sensitization, IgE and IgG, innate or adaptive cytokine production, eNO). EHAAS has longitudinally evaluated parental and child perceived stress, life events, socioeconomic stressors, and their associations with wheeze and immune responses. |
494 |
Diane Gold |
Boston, MA |
| Infant Immune Study |
IIS |
The Infant Immune Study (IIS), led by Anne Wright and Fernando Martinez, (University of Arizona, Tucson), enrolled 482 newborns and their families between 1996-2004 with the goal of exploring immune system markers of the early life origins of asthma in a population-based, non-selected, prospective birth cohort study. Two of the strengths of the IIS study are the longitudinal biomarker measurements and the detailed data available for illnesses and infant feeding practices during the first year of life. Environmental exposures assessed in infancy include indoor dogs, day care, siblings, tobacco smoke, air pollution (US EPA National Air Toxics Assessment), and house dust samples. All home addresses were collected prospectively and geocoded to link with air pollution data. |
482 |
Anne Wright and Fernando Martinez |
Tucson, AZ |
| Infant Susceptibility to Pulmonary Infections and Asthma Following RSV Exposure |
INSPIRE |
The Infant Susceptibility to Pulmonary Infections and Asthma Following RSV Exposure (INSPIRE) study led by Tina Hartert (Vanderbilt University, Nashville TN) is a prospective population-based non-selected birth cohort of 1,952 infants enrolled in the first few months of life in 2012-2014. INSPIRE study families are located throughout nine counties in Tennessee representing suburban, urban and rural areas of the state. The goals are to identify and understand the effects of early-life respiratory illnesses and microbial colonization on the subsequent development of childhood asthma. Environmental assessments in early life include viral diagnostics, pets, stress and behavior, household characteristics, bacterial lipopolysaccharides (LPS), personal microbiome, and dietary information. Extensive phenotyping and genotyping data include immune response to infection, SPT, wheezing, and genome-wide association studies (GWAS); follow-up is ongoing. |
1946 |
Tina Hartert |
Nashville, TN |
| Microbes, Allergy, Asthma and Pets |
MAAP |
The Microbes, Allergy, Asthma and Pets (MAAP) study led by Edward Zoratti (Henry Ford Health, Detroit MI) was established in 2014 as a birth cohort designed to determine whether keeping dogs in the home influences early-life immune development, infants’ intestinal microbiota, and the risks of allergic diseases and asthma. The study enrolled 120 mothers and their newborns, half of whom lived with indoor dogs during the first 18 months of life and half in pet-free homes. Environmental samples include peripartum maternal vaginal swabs for microbiome analysis, household characteristics, dust sampling, infant and parental stool and skin microbiome, infant oral microbiome, parental total and specific IgE, blood, and immune studies (dendritic cell, Treg and basophil markers and peripheral blood mononuclear cell [PBMC] stimulated cytokine responses). DNA, RNA and serum/plasma samples have been banked. |
141 |
Edward Zoratti |
Detroit, MI |
| Tucson Children’s Respiratory Study |
TCRS |
10. The Tucson Children’s Respiratory Study (TCRS) led by Fernando Martinez and Anne Wright (University of Arizona) was established in 1980 as a prospective, non-selected birth cohort. The participants (initial n=1246) have passed their fourth decade, offering a unique opportunity to investigate the risk factors for and the potential disease mechanisms involved in the early origins of asthma and chronic obstructive pulmonary disease (COPD). Exposures assessed in infancy included: indoor dogs, day care, siblings, tobacco smoke and air pollution. Samples collected include DNA and serum, and longitudinal assessments of lung function are continuing. Complete address histories have been geocoded to link with archived air pollution data (NO2, PM2.5 and PM10) from the 1980s. |
1246 |
Fernando Martinez and Anne Wright |
Tucson, AZ |
| Urban Environment and Childhood Asthma |
URECA |
The Urban Environment and Childhood Asthma (URECA) study led by James Gern (University of Wisconsin–Madison) is a high-risk birth cohort study (n=609) started in 2004 at four urban centers selected for high rates of poverty and asthma morbidity (Baltimore, Boston, New York City, St. Louis; Inner City Asthma Consortium). The goals are to identify early life environmental factors in urban settings that affect immune development, wheezing illnesses, and asthma. Environmental assessments include maternal stress and depression, pollutants (NO2, urinary cotinine), respiratory viruses (well child visits and during illness), house dust (microbiome, allergens, endotoxin), and questionnaires. Outcomes include lung function (spirometry, oscillometry) beginning at age 3 years, immune development (CBMC and PBMC cytokine responses), allergic sensitization (serum IgE and skin testing), food allergy, atopic dermatitis, wheezing illnesses and asthma. DNA, RNA (from PBMC) and serum/plasma samples have been banked. |
609 |
James Gern |
Baltimore, MD; Boston, MA; New York, NY; St. Louis, MO |
| Wayne County Health Environment Allergy and Asthma Longitudinal Study |
WHEALS |
The Wayne County Health Environment Allergy and Asthma Longitudinal Study (WHEALS) led by Christine Johnson (Henry Ford Health, Detroit MI) is a population-based birth cohort in Detroit and Western Wayne County suburbs to examine the relationships between early life exposures such as pets, infections and the environmental and infant gut microbiome in relationship to the development of allergic diseases. Samples include house dust, infant stool, blood (including cord blood), and assessments of total IgE, specific IgE (sIgE) and SPT to 10 common allergens. Clinic visits at 10-11 years of age measured eNO, cytokines, eosinophils, neutrophils, total and allergen-specific IgE, spirometry with albuterol challenge, and methacholine challenge. |
1258 |
Christine Johnson |
Detroit, MI |
| Wisconsin Infant Study Cohort |
WISC |
The Wisconsin Infant Study Cohort (WISC) study led by James Gern (University of Wisconsin–Madison) and Christine Seroogy (University of Wisconsin–Madison) is a birth cohort started in 2014 and being conducted in rural Wisconsin (Marshfield area) that enrolled 100 infants born into dairy farm families and an equal number born into rural non-farm families. The goals are to identify prenatal and early life exposures that affect immune development and respiratory illnesses in infancy. Environmental assessments include maternal prenatal health and medications, microbial exposures (settled dust from home and barn, vacuumed dust from the home, tap water, raw cow milk [if consumed], breast milk, maternal vaginal swab), and microbial colonization (skin swab, saliva, stool, nasal mucus). Other assessments/samples include respiratory viruses, atopic dermatitis, serum, blood cells, urine, DNA, and blood RNA. Outcome measures include respiratory illnesses, allergic sensitization, and wheezing illnesses. |
311 |
James Gern and Christine Seroogy |
Madison, WI |